Medicare Provider Credentialing & Enrollment 102 : Guide To Enrollment and Credentialing
$199.00 – $299.00
Session Overview
This is the second installment in our Credentialing and Enrollment webinar series. In this in-depth session, Yesenia leads a comprehensive training designed to equip you with the knowledge and tools needed to successfully credential both physicians and mid-level providers. The webinar walks you through every step of the credentialing process, offering customizable templates for application cover letters, required documentation checklists, CV guidelines, and more. You’ll also receive tools to assist with document tracking and payer application status monitoring.
Topics Covered
-
Documentation requirements for providers
-
Verification and validation of provider documents
-
Systems for tracking documentation
-
Organizing and maintaining provider records
-
Managing CAQH, PECOS, NPPES, and I&A accounts
-
Creating and managing provider portal profiles
-
Preparing and submitting payer applications
-
Enrollment requirements and details for various payers
-
Tracking the status of payer applications
-
Medicare and Medicaid enrollment processes
-
Linking providers to payers
-
Best practices for timely and effective communication
-
Final steps once payer approval is granted
-
Access to printable, customizable forms, letters, and tracking tools
-
Live Q&A session
Learning Goals
-
Set up and manage CAQH, PECOS, NPPES, and I&A profiles
-
Complete payer enrollment forms accurately
-
Understand the follow-up process for submitted applications
-
Navigate payer-specific submission requirements
-
Identify key contacts and submission guidelines for each payer
-
Effectively track the status of enrollment application packages
Focus Areas
-
CMS PECOS
-
Medicare enrollment and revalidation
-
Durable Medical Equipment (DME) credentialing
-
Mental health provider credentialing (e.g., LCPC, LMFT)
-
Rural Health Clinics (RHCs), Hospitals, and RHEs
-
MACs and CHOW processes
-
Ownership and organizational data requirements
-
NPI profile setup
-
CAQH and workflow management
-
EFT, credentialing, and provider enrollment best practices
Ideal Participants
This webinar is designed for professionals involved in provider credentialing and enrollment, including:
-
Practice Managers
-
Credentialing Specialists (PESC, CPMSM)
-
Revenue Cycle Managers
-
Directors and CFOs
-
Operations Leaders
-
EFT and Enrollment Coordinators
| Session Type |
Live ,Recording ,Transcript ,Live + Recording ,Transcript + Recording ,Live + Transcript |
|---|
Related products
Physician Employment Agreements: Problem Areas that can be Landmines
| Session Type |
Live ,Recording ,Transcript ,Live + Recording ,Transcript + Recording ,Live + Transcript |
|---|
Mastering Provider-Based Hospital Outpatient Billing & Supervision in 2025
| Session Type |
Live ,Recording ,Transcript ,Live + Recording ,Transcript + Recording ,Live + Transcript |
|---|
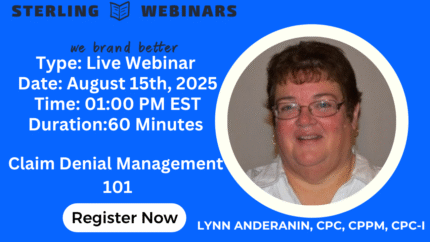
2025 Claim Denial Management 101: Turn Lost Revenue into Practice Profit
| Session Type |
Live + Transcript ,Live ,Recording ,Transcript ,Live + Recording ,Transcript + Recording |
|---|
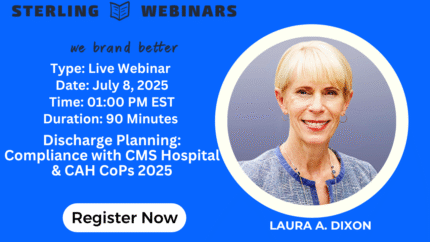
Discharge Planning: Compliance with CMS Hospital & CAH CoPs 2025
| Session Type |
Transcript ,Live + Recording ,Transcript + Recording ,Live + Transcript ,Live ,Recording |
|---|
CMS Hospital Restraint and Seclusion: Navigating the Most Problematic CMS Standards 2025
| Session Type |
Transcript ,Live + Recording ,Transcript + Recording ,Live + Transcript ,Live ,Recording |
|---|
Emergency Services, Emergency Procedures and EMTALA Obligations: CMS Hospital Conditions of Participation 2025
Medicare Provider Credentialing & Enrollment 101: Guide To Enrollment and Credentialing
| Session Type |
Live + Transcript ,Live ,Recording ,Transcript ,Live + Recording ,Transcript + Recording |
|---|








Reviews
There are no reviews yet.